Mole Removal Explained: From Diagnosis to Treatment
Everything you need to know about mole removal.
At Dermatology North Sydney, we understand that mole removal can be a concern for many of our patients. Whether you’re seeking cosmetic removal or have concerns about a potentially problematic mole, our team of specialists is here to guide you through the process. We offer a range of mole removal techniques, including surgical excision and laser removal, tailored to meet your specific needs and ensure your comfort throughout the procedure.
In this comprehensive guide, we’ll walk you through the journey of mole removal, from initial diagnosis to aftercare. We’ll explore different types of moles, including nevus and angiomas, and discuss various removal methods such as liquid nitrogen treatment and mole removal surgery. Our goal is to provide you with the information you need to feel confident and well-informed about your mole removal options, whether you’re dealing with a flat mole or a more complex skin issue.
Understanding Moles and Their Types
Moles, also known as nevi, are common skin growths that develop when pigment-producing cells (melanocytes) grow in clusters. They can appear anywhere on the body and vary in colour, shape, and size. While most moles are harmless, it’s important to understand the different types to recognize any potential signs of skin cancer, such as melanoma.
1. Common moles
Common moles, or acquired nevi, typically appear during childhood or adolescence. They are usually round or oval, with a smooth surface and distinct edges. Common moles tend to be uniform in colour, ranging from light to dark brown, and are generally less than 6mm in diameter. These moles are usually benign and do not require treatment unless they become irritated or are cosmetically undesirable.
2. Atypical moles
Atypical moles, also known as dysplastic nevi, are unusual-looking moles that may share some features with melanoma. They are often larger than common moles (>6mm), with irregular borders and a mix of colours, including shades of brown, tan, or pink. Atypical moles can be flat or raised and may have a pebbly surface. While atypical moles are not cancerous, having multiple atypical moles increases your risk of developing melanoma. Regular skin checks and mole monitoring are crucial for early detection and prevention.
3. Congenital moles
Congenital moles are present at birth or develop within the first year of life. They can vary in size, from small to giant (>20 cm in adulthood). Congenital moles may be raised or flat, with a smooth or rough surface, and can have hair growing from them. The colour of these moles can range from light brown to black. Larger congenital moles have a higher risk of developing into melanoma, so close monitoring and regular skin checks are essential.
4. Other types of moles include:
- Halo nevi: Moles surrounded by a white ring of depigmented skin
- Blue nevi: Deeply pigmented, blue-grey moles that occur due to melanocytes in the deeper layers of the skin
- Spitz nevi: Pink, raised moles that can resemble melanoma but are generally benign
If you notice any new, changing, or unusual moles, it’s important to have them evaluated by a dermatologist. Mole removal techniques, such as surgical excision or cosmetic removal using lasers or liquid nitrogen, can be used to remove suspicious or bothersome moles. Remember, early detection is key in preventing skin cancer, so regular self-examinations and professional skin checks are crucial for maintaining healthy skin.

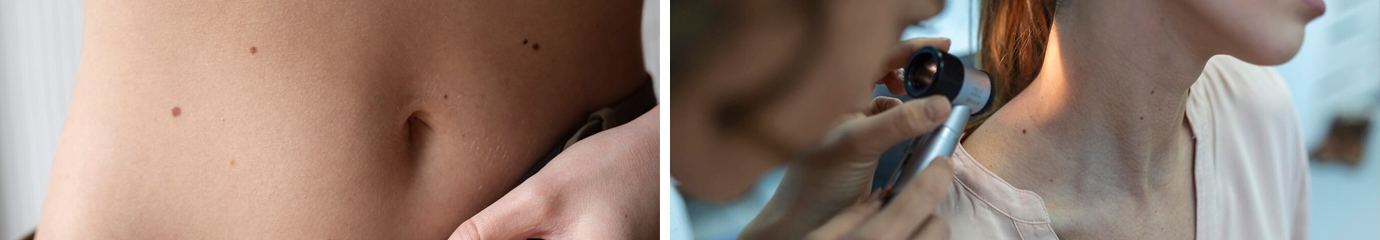
Diagnosing Moles
At Dermatology North Sydney, our skilled dermatologists employ a comprehensive approach to diagnose moles and determine whether they require mole removal. The diagnostic process involves a thorough visual examination, advanced techniques like dermoscopy, and, when necessary, a biopsy to confirm the nature of the mole.
Visual examination
The first step in diagnosing a mole is a careful visual assessment by one of our experienced dermatologists. They will examine the mole’s size, shape, colour, and texture, as well as any signs of asymmetry or irregular borders. Our dermatologists also consider the location of the mole and compare it to other moles on your body to identify any unusual or atypical characteristics. This initial evaluation helps determine whether the mole is likely to be benign (non-cancerous) or if it warrants further investigation.
During the visual examination, our dermatologists may ask about any changes you’ve noticed in the mole, such as growth, itching, or bleeding. They will also inquire about your medical history, including any previous skin cancers or family history of melanoma. This information, combined with the physical appearance of the mole, guides the next steps in the diagnostic process.
Dermoscopy
Dermoscopy is a non-invasive technique that allows our dermatologists to examine moles in greater detail using a specialised magnifying instrument called a dermatoscope. This tool provides a clear, illuminated view of the mole’s structure and pigmentation patterns beneath the skin’s surface. Dermoscopy enhances the accuracy of mole diagnosis and helps distinguish between benign moles, such as angiomas or nevus, and potentially cancerous lesions.
Our dermatologists are highly trained in the use of dermoscopy and follow established algorithms to assess moles systematically. They look for specific features, such as irregular pigment networks, asymmetrical patterns, and blue-white structures, which may indicate the presence of melanoma. Dermoscopy is particularly valuable in evaluating flat moles, as it allows for a more detailed analysis of their characteristics.
Biopsy
In some cases, a biopsy may be necessary to confirm the diagnosis of a suspicious mole. During a biopsy, our dermatologists remove either a small sample (punch biopsy) or the entire mole (excisional biopsy) for microscopic examination by a pathologist. This procedure is typically performed under local anaesthesia to minimise discomfort.
The decision to perform a biopsy is based on the dermatologist’s assessment of the mole’s clinical and dermoscopic features. Moles that exhibit warning signs, such as asymmetry, irregular borders, colour variations, or a diameter larger than 6mm, are more likely to require a biopsy. Additionally, any mole that has undergone recent changes or is causing symptoms like itching or bleeding may warrant a biopsy to rule out skin cancer.
The biopsy results provide a definitive diagnosis, confirming whether the mole is benign or malignant. If the mole is found to be cancerous, the biopsy also helps determine the type and stage of the skin cancer, which is crucial for developing an appropriate treatment plan. In cases where melanoma is diagnosed, our dermatologists work closely with you to discuss the next steps, which may include further surgical excision or additional tests to assess the extent of the disease.
At Dermatology North Sydney, we understand that undergoing a mole biopsy can be a source of anxiety for many patients. Our compassionate team is dedicated to providing a supportive environment and guiding you through the process with clear explanations and personalised care. We prioritise your comfort and well-being throughout the diagnostic journey, ensuring that you receive the highest standard of care and support.
Mole Removal Techniques
At Dermatology North Sydney, we offer several effective mole removal techniques tailored to your specific needs. Our skilled dermatologists will guide you through the process, ensuring optimal results and minimal scarring. Let’s explore the most common mole removal methods:
Surgical excision
Surgical excision is a precise technique that involves removing the entire mole and a small margin of surrounding skin using a scalpel. This method is particularly useful for larger moles or those suspected of being cancerous. Our dermatologists numb the area with local anaesthesia before carefully excising the mole. The wound is then closed with sutures, which are typically removed after 7-14 days, depending on the location. Surgical excision allows for a complete removal of the mole and provides a sample for histopathological analysis to rule out any malignancy.

While surgical excision may result in a linear scar, our skilled dermatologists use advanced techniques to minimise scarring and ensure the best cosmetic outcome. We provide comprehensive aftercare instructions to promote proper healing and reduce the risk of complications.
Shave excision
Shave excision is a quick and effective method for removing raised moles or those with a small base. This technique involves numbing the area with local anaesthesia and using a sharp razor to carefully shave off the mole at skin level. Our dermatologists may also use an electrode to feather the edges of the excision site, blending it with the surrounding skin for a more seamless appearance.
Shave excision is an excellent option for cosmetic mole removal, as it typically results in minimal scarring. The procedure is performed in our office and requires no stitches, allowing for a faster recovery time. After the mole is removed, a scab will form over the area, which will naturally fall off within a few days to reveal new, healthy skin.
Laser removal
Laser mole removal is a non-invasive alternative to traditional surgical techniques. This method uses targeted laser energy to break down the pigment cells within the mole, causing it to gradually fade away. Our dermatologists use state-of-the-art laser technology to precisely target the mole while minimising damage to the surrounding skin.
Laser mole removal is particularly effective for flat, pigmented moles such as angiomas or nevus. The procedure is performed in our office and requires no anaesthesia or downtime. Most patients experience minimal discomfort during the treatment, describing it as a slight snapping or burning sensation.
Multiple laser sessions may be necessary to achieve optimal results, depending on the size, depth, and colour of the mole. Our dermatologists will develop a personalised treatment plan to ensure the best possible outcome for your unique needs.
It’s important to note that while laser mole removal is a safe and effective option for many patients, it may not be suitable for all types of moles. Our dermatologists will thoroughly evaluate your mole and discuss the most appropriate treatment options during your consultation.
At Dermatology North Sydney, we prioritise your safety and satisfaction. Our experienced dermatologists use the latest techniques and technologies to provide the highest quality care for all your mole removal needs. Whether you opt for surgical excision, shave excision, or laser removal, you can trust our team to deliver exceptional results with minimal scarring and downtime.
If you’re considering mole removal for cosmetic reasons or due to medical concerns, schedule a consultation with our skilled dermatologists today. We’ll work with you to develop a personalised treatment plan that addresses your unique needs and goals, ensuring a confident and healthy appearance.
Aftercare and Recovery
At Dermatology North Sydney, we prioritise your comfort and well-being throughout the mole removal process, including the crucial aftercare and recovery period. Our experienced dermatologists will provide you with detailed instructions to ensure proper healing and minimise the risk of complications. Let’s explore the key aspects of post-mole removal care.
Wound care
Proper wound care is essential for promoting healing and reducing the risk of infection. After your mole removal procedure, we will apply a sterile dressing to protect the treated area. It’s important to keep the dressing clean and dry for the first 24-48 hours. Avoid getting the wound wet during this time, and follow our instructions for changing the dressing as needed.
When cleaning the wound, use a gentle, fragrance-free cleanser and lukewarm water. Pat the area dry with a clean, soft towel, and apply a fresh dressing as directed. Avoid using alcohol, hydrogen peroxide, or harsh chemicals on the wound, as these can irritate the skin and delay healing.
Potential complications
While complications after mole removal are rare, it’s important to be aware of potential issues and contact us promptly if you experience any of the following:
- Excessive bleeding or oozing from the wound
- Increasing pain, redness, swelling, or warmth around the treated area
- Discharge of pus or foul-smelling fluid from the wound
- Fever or chills, which may indicate an infection
Our team will work with you to address any complications and ensure proper healing.
Follow-up appointments
We will schedule follow-up appointments to monitor your healing progress and address any concerns you may have. These appointments are crucial for ensuring that the wound is healing properly and that there are no signs of infection or other complications.
During your follow-up visits, we will assess the wound, change dressings if necessary, and provide guidance on scar management. We may recommend specific products or techniques to minimise scarring and promote optimal healing.
In addition to wound care, it’s important to protect the treated area from sun exposure during the healing process. Use a broad-spectrum sunscreen with an SPF of at least 30 and cover the area with protective clothing when outdoors. Sun exposure can cause hyperpigmentation and may worsen the appearance of scars.
As you heal, you may experience some itching or mild discomfort around the treated area. Resist the urge to scratch or pick at the wound, as this can introduce bacteria and increase the risk of infection. If itching persists, contact our office for guidance on safe relief options.
Rest assured that our team at Dermatology North Sydney is here to support you throughout the aftercare and recovery process. We are committed to providing the highest quality care and ensuring that you achieve the best possible results from your mole removal procedure. If you have any questions or concerns during your recovery, don’t hesitate to reach out to us for assistance.
Conclusion
Mole removal is a common procedure that has a significant impact on both health and appearance. From understanding different types of moles to exploring various removal techniques, this guide aims to provide a comprehensive overview to help patients make informed decisions. The journey from diagnosis to treatment involves careful examination, advanced diagnostic tools, and personalised care to ensure the best possible outcomes.
At Dermatology North Sydney, we’re committed to deliver top-notch care throughout the mole removal process. Our skilled team uses cutting-edge techniques to remove moles safely and effectively, while prioritising patient comfort and minimising scarring. Remember, regular skin checks and prompt attention to any changes in moles are key to maintain healthy skin and catch potential issues early. If you have concerns about a mole or are considering removal, don’t hesitate to reach out to a dermatologist to discuss your options.
FAQs
What should I know before having a mole removed?
Before your mole removal appointment, it’s important to examine your skin yourself. Look for signs that could indicate melanoma by remembering the ABCs: Asymmetry (where the two halves of the mole do not match), and any other unusual changes in your moles. Make a note of these observations to discuss with your dermatologist.
What care is required after a mole is removed?
Post-mole removal, your healthcare provider will typically apply petroleum jelly (such as Vaseline®) to the affected area and cover it with a bandage. It is crucial to keep the area moist with the jelly and clean it daily for a few days following the procedure.
How are moles diagnosed and removed?
Moles are usually diagnosed during a full skin examination by a healthcare professional, who will assess your skin from head to toe. If there is any suspicion of cancer, the mole will be removed and sent for a biopsy, where it is examined under a microscope to check for cancer cells.
How long does the site of mole removal need to be kept covered?
After mole removal, you might experience slight soreness at the site for about 1 to 4 days. It’s important to keep the area clean and covered with a bandage for 1 to 2 days to ensure it is protected while it begins to heal.

